Choosing the right E/M level should feel clear, not confusing. This guide shows you how to pick the correct level without overcoding or undercoding. We focus on real clinic work, not theory. You will learn how to use medical decision making or total time, what to document in plain language, and how to avoid denials. Each section gives simple steps you can apply on your next visit.
You will see short examples, quick rules you can trust, and phrases you can drop into the note. The goal is simple. Match your code to the care you provided, keep your claims clean, and move on with your day.
In This Blog, We Will Cover:
- Pick your code basis first
- Quick refresher on E/M office codes
- Medical decision making made simple
- Using time the right way
- Prolonged services without confusion
- Common real life visit paths
- Independent interpretation that helps your level
- Independent historian and social drivers
- Preventive visit plus problem visit
- E/M with a minor procedure on the same day
- Five minute E/M decision path
- One minute checklist before you sign
- Conclusion
Pick your code basis first
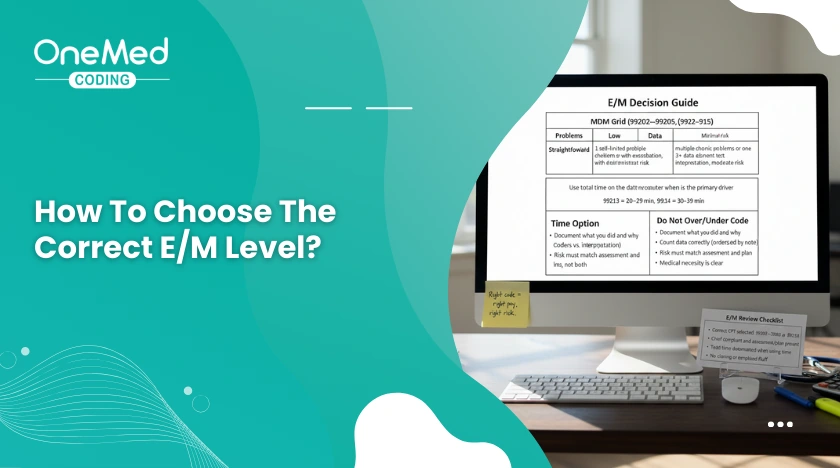
Choose one method for the visit. Use Medical Decision Making or total time. Do not mix them.
Use MDM when the visit is driven by clinical thinking and decisions. You worked on problems, reviewed data, and made management choices.
Use total time when counseling and care coordination took most of the visit and your minutes meet a code’s range.
One line to make it clear
- “E/M level chosen by MDM.”
- or
- “E/M level chosen by total time. 32 minutes today.”
Quick refresher on E/M office codes
New patient visits use 99202 to 99205.
Established patient visits use 99212 to 99215.
You may select the level by MDM or by total time on the date of service. Higher levels reflect more complex decisions or more time.
Medical decision making made simple
MDM shows the thinking you did to treat the patient today. It has three parts. Problems addressed, data you reviewed, and risk from your plan.
Problems addressed
Count only conditions you evaluated or managed today. Write status in plain words, such as stable, worsening, or new.
Example line: “Type 2 diabetes not at goal, added metformin, follow up in two weeks.”
Data you review and analyze
Note orders, results you reviewed, outside notes, or your own test interpretation. Avoid double counting.
Example line: “Reviewed labs from last week, personally interpreted EKG, no ST changes.”
Risk from management
Show decisions that carry risk, like starting or changing prescription drugs, ordering tests with risk, urgent referrals, or sending the patient to the ER. Social factors that change the plan can also increase risk.
Example line: “Started antibiotic, counselled on side effects, return precautions given.”
Quick guide to levels
- Straightforward: self limited problem, minimal data, no Rx change.
- Low: stable chronic illness or acute uncomplicated issue, limited data.
- Moderate: new problem with uncertain course or chronic illness with a flare, prescription drug management, or your own test interpretation.
- High: high risk decisions, severe illness, drug therapy with intensive monitoring, decision for hospitalization or ER transfer
Using time the right way
Use total time when counseling and care coordination dominate the day. Add up only your own work on the date of service, then select the code that matches the range.
What time includes on the date of service
Reviewing records for today’s visit, seeing the patient and counseling, ordering tests or meds, coordinating care, documenting the visit, and communicating with other clinicians about this patient.
What time does not include
Staff time, rooming, work on a different date, services you bill separately, travel time, or office admin work.
Time ranges at a glance
New patient
- 99202: 15–29 minutes
- 99203: 30–44 minutes
- 99204: 45–59 minutes
- 99205: 60–74 minutes
Established patient
- 99212: 10–19 minutes
- 99213: 20–29 minutes
- 99214: 30–39 minutes
- 99215: 40–54 minutes
One line to document
“Level chosen by total time. 28 minutes today for review, counseling, coordination, and documentation.”
Prolonged services without confusion
Add a prolonged service code only when your total time passes the top level time threshold for that visit type on the same date, and your payor allows the add on.
One line to document
“Prolonged service added. Total time 78 minutes today, beyond highest level range, for counseling, coordination, and documentation.”
Common real life visit paths
Acute cough with OTC plan
Likely level: 99212 or 99213 by MDM or time.
Why: Self limited problem, no tests, simple plan.
Note phrase: “Acute cough, no red flags, OTC meds advised, return if worse.”
Stable hypertension follow up
Likely level: 99213 by MDM.
Why: Chronic illness stable, routine labs, refill.
Note phrase: “HTN stable, reviewed BP log, refill lisinopril, labs ordered.”
Diabetes with medication change
Likely level: 99214 by MDM.
Why: Chronic illness not at goal, drug change, labs, close follow up.
Note phrase: “T2DM not at goal, increased metformin, A1C and CMP ordered, follow up two weeks.”
Chest pain same day workup
Likely level: 99214 or 99215 by MDM.
Why: New problem with uncertain prognosis, higher risk decisions.
Note phrase: “New chest pain, EKG read by me, no ST changes, cardiology referral, ER precautions given.”
Independent interpretation that helps your level
When you personally read a test and record a brief note, it counts toward MDM data if you are not billing a separate interpretation.
What to write
“Personally interpreted EKG, normal sinus rhythm, no ST changes, plan outpatient follow up.”
or
“Personally reviewed chest X ray, no focal consolidation, continue current treatment.”
Independent historian and social drivers
Use this when someone other than the patient gives key history, or when social factors change your plan. An independent historian adds data. Social drivers, like cost limits or no refrigeration for insulin, can increase risk because they change management.
What to write
“Independent historian, mother supplied history due to child’s age.”
or
“Social driver, cannot afford inhaler, switched to covered option and set delivery.”
Preventive visit plus problem visit
You may bill a preventive visit and a problem oriented E/M on the same day when the problem is separate and significant. Keep distinct documentation for the problem work and include a clear assessment and plan.
Quick guardrail
If the problem work is minor and fully addressed inside the preventive service, do not add a problem E/M.
E/M with a minor procedure on the same day
Bill an E/M with a minor procedure only when the evaluation is separate and significant. The E/M must be beyond the usual pre and post work for the procedure.
Simple test for modifier 25
Would you still have done the E/M if the procedure were not performed today? If yes, the E/M may be separate.
Note phrase: “Separate and significant E/M for new problem, procedure performed for different issue.”
Five minute E/M decision path
- Pick MDM or time for this visit.
- If MDM, list problems addressed, data you reviewed, and risk from your plan.
- If time, total your minutes and make sure they are all on the date of service.
- Check if prolonged time applies.
- If a procedure is done, decide if the E/M is truly separate.
- Write one clear sentence that shows why you chose the level.
One minute checklist before you sign
- Did I pick MDM or time
- If MDM, did I show problems, data, and risk
- If time, did I write total minutes and what I did today
- Did I include independent interpretation or independent historian when used
- If billed with a procedure or preventive, did I explain why it is separate
Conclusion
Right coding comes from clear choices and clean notes. Start by picking MDM or time. Show the problems you worked on, the data you touched, and the risk from your plan, or write a total minute count that matches a code range. Use the example phrases to keep it brief and clear. If you want a quick review of two sample notes, send them, and we will map each one to the correct level with a short checklist you can reuse.





0 Comments