Choosing the primary diagnosis should be simple, clear, and defensible. The primary diagnosis tells the payor why the patient was seen. If it is wrong, you risk denials, delays, or audits. If it is too aggressive, you risk overcoding. The goal is to match the doctor’s note to the most accurate reason for the visit, without stretching the code to something the record does not support.
We will cover the following topics:
- What the primary diagnosis means in plain language
- Why it matters for payments and compliance
- Core rules to avoid overcoding
- A step by step checklist to pick the right code
- How to handle tricky situations
- Documentation that proves medical necessity
- Working smart with EHR templates and prompts
- Quick internal audits and simple metrics
- Common examples across specialties
- A short do and do not list
- Conclusion
What the primary diagnosis means in plain language
The primary diagnosis is the main reason for the visit. It is the condition that drove the work, testing, or treatment today. If a patient came in for ear pain and the assessment shows acute otitis media, that infection is the primary diagnosis. Secondary diagnoses are extra problems that also matter, such as diabetes or hypertension, but they were not the main reason for today’s care.
Why it matters for payments and compliance
The primary diagnosis supports medical necessity. Medical necessity means the service makes sense for the problem treated. payors look at the code and the note side by side. If the code fits the story, claims move fast. If the code is too broad, too mild, or too severe for what is documented, it can cause a denial or a request for records. Getting the first code right reduces rework and keeps audits away.
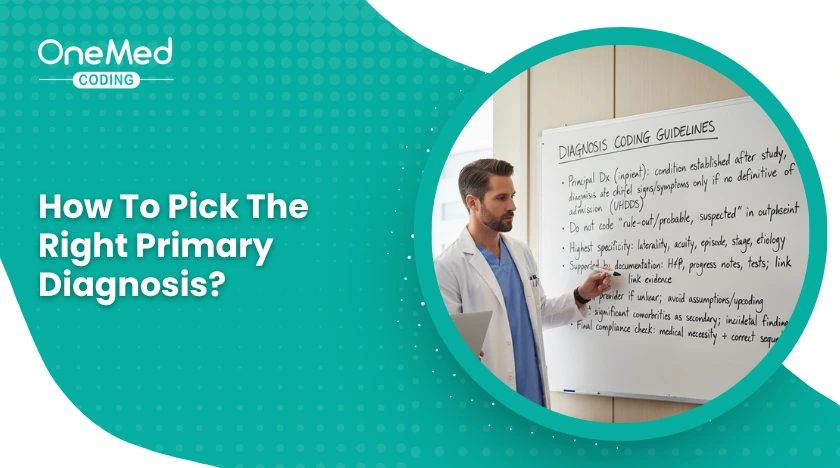
Core rules to avoid overcoding
- Code only what is known today; for outpatient visits do not code “rule out” or “probable”; use signs and symptoms if the diagnosis is not confirmed.
- Use the most specific code your note supports; include laterality and acute or chronic when documented, and do not guess when it is not.
- Link the diagnosis to the service; the note should show how the diagnosis connects to tests or treatment.
- Do not upcode severity; select severe or complicated codes only when the record clearly documents those features.
- Sequence correctly; list the main reason first, then other active conditions that affected care today.
A step by step checklist to pick the right code
- Read the chief complaint to know why the patient came in.
- Scan the assessment and plan to see what condition explains the complaint.
- Confirm certainty level and decide if it is a confirmed condition or still a symptom.
- Add detail such as laterality, acute or chronic, stage, and site.
- Check policy rules for any payor notes about coverage or linked tests.
- Review secondary conditions and add only those that affected today’s work.
- Match the code to the note and make sure the wording and code agree.
- Do a quick sanity check and ask if a reviewer would agree this is the main reason for the visit.
- Save a clear rationale with a short line in the plan for future reviewers.
How to handle tricky situations
Signs and symptoms only
If you cannot confirm a diagnosis today, code the symptom that brought the patient in, such as chest pain or cough. Add risk factors and relevant chronic conditions as secondary when they changed your workup.
Chronic disease with an acute flare
When a stable condition flares, code the acute flare as primary if that is the reason for extra work, and list the chronic condition as secondary. Example, asthma with acute exacerbation as primary, chronic asthma as secondary.
Injury and poisoning
Use the injury code first, including site and laterality if possible. Add external cause codes only if your clinic and payor require them. They explain how the injury happened, such as a fall.
Postoperative problems
If the visit is for a complication of surgery, code the complication first and name the link to the recent procedure in the note.
Screening and preventive visits
For pure screening, use screening codes. If the doctor finds something significant and treats it, the finding can become the primary diagnosis for the treatment part of the encounter.
Pregnancy and newborns
Follow the pregnancy or perinatal chapters for accurate sequencing. If your clinic does not manage pregnancy, refer and document the concern, then code the finding that led to referral.
Social factors that affect care
When housing, food, or transportation problems change care plans, include the related Z codes as secondary. They do not replace the medical reason for the visit, but they explain added work.
Documentation that proves medical necessity
Write in plain language. In the assessment and plan, include three simple pieces:
- What do you think the condition is? If not confirmed, state the key symptom.
- Why do you think that? List the findings that support the diagnosis and its severity.
- What are you doing? Document tests, treatment, and follow-up tied to the problem.
Example line, “Acute sinusitis, right side, ten days of congestion and facial pain, maxillary tenderness, starting amoxicillin, return if fever or worsening.”
Working smart with EHR templates and prompts
Templates save time, but they can push extra terms that inflate severity. Keep templates short. Turn off default phrases that do not apply to most visits. Use diagnosis picklists that include your most common, specific codes, such as laterality and acute versus chronic. Add prompts for key details, like “right or left,” “initial or subsequent,” and “with or without complications.” These little nudges prevent overcoding and undercoding.
Quick internal audits and simple metrics
Run a light audit each month. Pull ten charts per provider, or a fixed percent of visits, and check:
- Is the primary diagnosis the clear reason for the visit.
- Is the code as specific as the note allows.
- Were secondary conditions used only when they affected care.
- Do orders and treatments match the diagnosis.
Track two metrics on a simple dashboard. First pass acceptance rate for claims, and diagnosis related denials. If denials for “not medically necessary” or “diagnosis inconsistent with procedure” rise, review the notes and fix upstream.
Common examples across specialties
Primary care
Sore throat becomes strep pharyngitis when confirmed, otherwise code sore throat as the symptom and document the test plan.
Cardiology
Chest pain remains chest pain if acute coronary syndrome is not yet confirmed. If a confirmed diagnosis exists, such as unstable angina, use that.
Orthopedics
Right knee pain from osteoarthritis can be coded as unilateral primary osteoarthritis, right knee, when documented. If you only know “knee pain,” code the symptom and plan.
Dermatology
For a lesion removal, code the confirmed lesion type if pathology is back. If not, code the lesion by site and size, and add pathology pending in the note.
Behavioral health
If a specific disorder is diagnosed and documented, use it. If evaluation is ongoing, code the presenting symptom such as anxiety, and describe the plan.
A short do and do not list
Do
- Code the condition that best explains today’s work.
- Use the highest specificity supported by the note.
- Add secondary diagnoses only when they changed evaluation or treatment.
- Keep a simple checklist at the coder desk and in provider rooms.
Do not
- Guess at severity or laterality.
- Use “rule out” diagnoses in outpatient settings.
- List every chronic condition if it did not affect today’s care.
- Let templates add findings that are not true for this patient.
Conclusion
The right primary diagnosis is the one that matches the story in the record. Read the complaint, confirm what is known today, pick the most specific code that fits the note, and show the link to your plan. When in doubt, choose the symptom rather than a not yet proven condition. Use brief checklists, smart EHR prompts, and light monthly audits to keep everyone on track. These small habits prevent overcoding, reduce denials, and keep your claims clean and defensible.





0 Comments